Differentiation of acquired white matter disorders
There are many conditions that cause acquired cerebral white matter damage, and I shall describe how to distinguish among them on the basis of cranial MRI findings in particular.
Among the important disorders that may cause acquired cerebral white matter damage are (1) brain tumors: malignant lymphoma, metastatic brain tumors, and gliomatosis cerebri; (2) cerebrovascular disease: Binswanger disease and amyloid angiopathy; (3) infections: Herpes simplex encephalitis and progressive multifocal leukoencephalopathy (PML); (4) poisoning or metabolic disorders: hypoxic encephalopathy, carbon monoxide (CO) poisoning, Marchiafava-Bignami disease, toluene poisoning, and drug-induced leukoencephalopathy; (5) autoimmune and inflammatory diseases: multiple sclerosis, neuromyelitis optica (NMO), and systemic lupus erythematosus (SLE); and (6) cerebral edema and hydrocephalus: posterior reversible encephalopathy syndrome (PRES) and normal-pressure hydrocephalus.
(1) Brain tumors
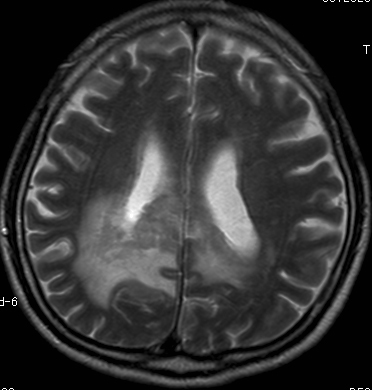
Malignant lymphoma (Figure 1): If the density of cells is high, lymphoma will appear hyperdense on cranial CT and hyperintense on T2-weighted cranial MRI in comparison with white matter, but with comparatively low signal intensity compared with the surrounding edema. Contrast enhancement is relatively uniform.
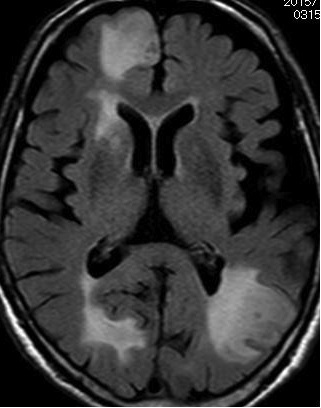
Metastatic brain tumors (Figure 2: A, FLAIR image; B, contrast-enhanced image): If multiple metastatic brain tumors are present, they and the surrounding edema cause widespread damage to the cerebral white matter. They are contrast-enhanced in the form of a ring or nodules.
Gliomatosis cerebri: The tumor expands in a diffuse manner along nerve fibers. If diffuse white matter degeneration is present but bilateral lesions are somewhat asymmetrical with a contrast effect or mass effect, a brain biopsy must be performed to reach a definitive diagnosis.1)
(2) Cerebrovascular disease
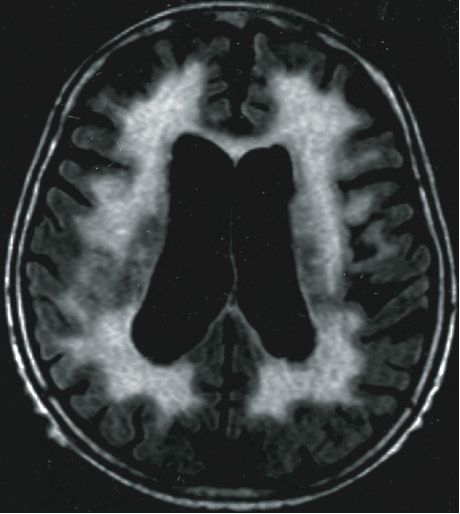
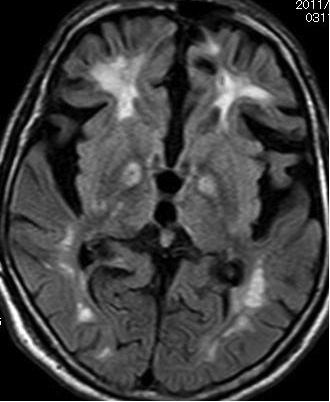
Binswanger disease (Figure 3): This is the cause of cerebrovascular dementia. Diffuse hyperintensity is evident on T2-weighted imaging. Small infarcts are often present in the basal ganglia. These imaging findings are very similar to those for cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy(CADASIL), which is caused by a mutation in the Notch3 gene, but CADASIL can be distinguished from Binswanger disease by the fact that the hyperintensity extends to the tip of the temporal lobe on T2-weighted imaging.2)
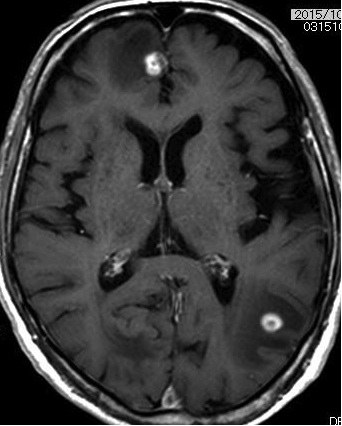
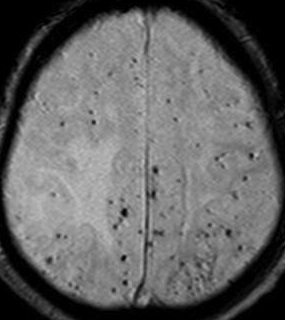
Cerebral amyloid angiopathy (Figure 4): Numerous microbleeds are visible in the cerebral and subcortical white matter on T2-weighted imaging. These microbleeds tend to occur in the occipital and temporal lobes.
(3) Infections
Herpes encephalitis: Diffusion-weighted imaging is useful for the early detection of lesions.3) If lesions form bilaterally, they exhibit left-right asymmetry. The basal ganglion is not normally damaged. Edema is predominantly evident in the cortex and subcortical white matter of the parietal lobe, insular gyri, cingulate gyri, and the inferior surface of the frontal lobe. Cerebral white matter lesions may appear within a few weeks or months of onset.4)
PML: This is a demyelinating encephalopathy caused by the John Cunningham (JC) virus that develops secondarily in immunocompromised patients. The subcortical white matter is damaged but the cortex is not, and the border between them is well-demarcated. It appears hypointense on T1-weighted imaging and hyperintense on T2-weighted and FLAIR imaging. No contrast enhancement effect is evident.
(4) Poisoning and metabolic disorders
Hypoxic encephalopathy: Diffusion-weighted imaging is useful for diagnosis. The hippocampus, cerebral white matter, basal ganglion, and other areas appear hyperintense on T2-weighted imaging.
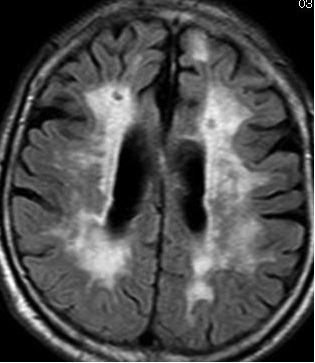
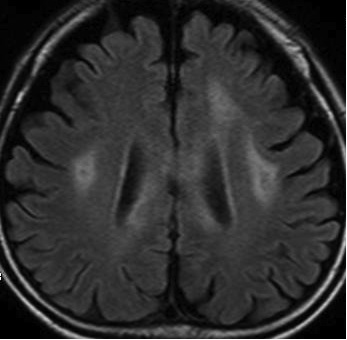
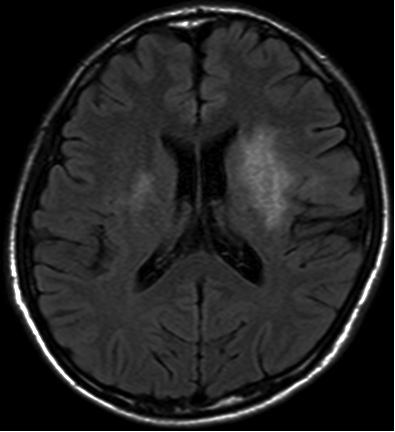
CO poisoning: Delayed diffuse demyelination. The bilateral cerebral white matter and globus pallidus appeared hyperintense on T2-weighted imaging (Figures 5 and 6).5)
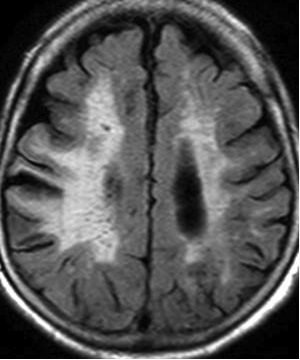
Marchiafava-Bignami disease: This disease occurs in individuals suffering from chronic alcohol poisoning or malnutrition. The enlarged corpus callosum appears hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging (Figure 7). Abnormal signals may also be observed in the cerebral white matter as well as the corpus callosum (Figure 8).
Toluene poisoning: Toluene is found in coatings and thinner. The cerebral white matter, middle cerebellar peduncle, brainstem, and other areas appear as bilaterally symmetrical hyperintensities on T2-weighted imaging.6)
Drug-induced leukoencephalopathy: Fluorouracil chemotherapy agents and other drugs may induce leukoencephalopathy. The cerebral white matter appears diffusely hyperintense on T2-weighted imaging.7)
(5) Autoimmune and inflammatory diseases
Multiple sclerosis: Multiple lesions appear at different times and in different locations, mainly in the cerebral white matter. These lesions are known as "ovoid lesions" or "Dawson's finger" because of their shape. During a relapse, the lesions are contrast-enhanced as a result of the breakdown of the blood-brain barrier by acute infection, and these contrast-enhanced lesions are nodular or ring-shaped. Nodular lesions are believed to represent severe inflammation with mild demyelination. The open-ring sign is useful in distinguishing this condition from brain tumors.
NMO: NMO tests positive for anti-aquaporin-4 antibody and is frequently associated with spinal cord lesions extending across three or more vertebrae, known as long cord lesions (LCLs), although in some cases cerebral white matter lesions resembling PRES may also be present among the NMO cerebral lesions.8) NMO cerebral lesions may exhibit cloud-like enhancement.9)
SLE (Figure 9): Central nervous system lesions caused by SLE are known as "CNS lupus." CNS lesions exhibit a wide variety of imaging findings, but cerebrovascular disturbance and demyelinated lesions may be apparent.10)
(6) Cerebral edema and hydrocephaly
PRES: The possible causes of this reversible edematous condition include hypertensive encephalopathy, eclampsia, and immunosuppressants. It exhibits vascular edema predominantly in the occipital or parietal lobe, appearing hyperintense on T2-weighted and FLAIR imaging with a high apparent diffusion coefficient (ADC).11)
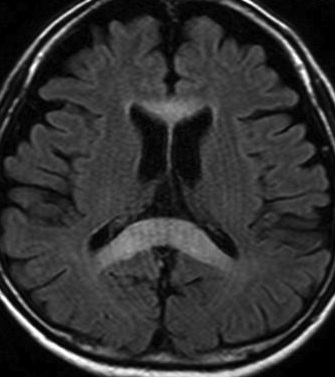
Normal-pressure hydrocephalus: Narrowing of the cerebral sulci in the high-convexity area of the brain and expansion of the fissure of Silvius are present, and the Evans index (the ratio of the maximum distance between the anterior horns of the bilateral lateral ventricles and the width of the intercranial cavity in the same cross-section) exceeds 0.3. Periventricular hyperintensity may also be visible on T2-weighted imaging.
(Dai MATSUI MD, Department of Neurology, Otsu Red Cross Hospital)
References
- Desclee P, Rommel D, Hernalsteen D et al: Gliomatosis cerebri, imaging findings of 12 cases. J Neuroradiol 37:148-158, 2010
- Tomimoto H, Ohtani R, Wakita H et al: Small artery dementia in Japan: radiological differences between CADASIL, leukoaraiosis and Binswanger’s disease. Dement Geriatr Cogn Disord 21:162-169, 2006
- McCabe K, Tyler K, Tanabe J: Diffusion-weighted MRI abnormalities as a clue to the diagnosis of herpes simplex encephalitis. Neurology 61:1015-1016, 2003
- Mitsufuji N, Ikuta H: Asymptomatic self-limiting white matter lesions in the chronic phase of herpes simplex encephalitis. Brain Dev 24:300-303, 2002
- O’Donnell P, Buxton PJ, Pitkin A, et al: The magnetic resonance imaging appearances of the brain in acute carbon monoxide poisoning. Clin Radiol 55:273-280, 2000
- Aydin K, Sencer S, Demir T et al: Cranial MR findings in chronic toluene abuse by inhalation. AJNR 23:1173-1179, 2002
- Fujikawa A, Tsuchiya K, Katase S et al: Diffusion-weighted MR imaging of Carmofur-induced leukoencephalopathy. Eur Radiol. 11:2602-2606, 2001
- Magana SM, Matiello M, Pittock SJ, et al: Posterior reversible encephalopathy syndrome in neuromyelitis optica spectrum disorders . Neurology 72:712-717, 2009
- Ito S, Mori M, Makino T et al: “Cloud-like enhancement” is a magnetic resonance imaging abnormality specific to neuromyelitis optica. Ann Neurol 66:425-428, 2009
- Jennings JE, Sundgren PC, Attwood J, et al: Value of MRI of the brain in patients with systemic lupus erythematosus and neurologic disturbance. Neuroradiology. 46:15-21, 2004
- Bartynski WS: Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. AJNR 29:1036-1042, 2008