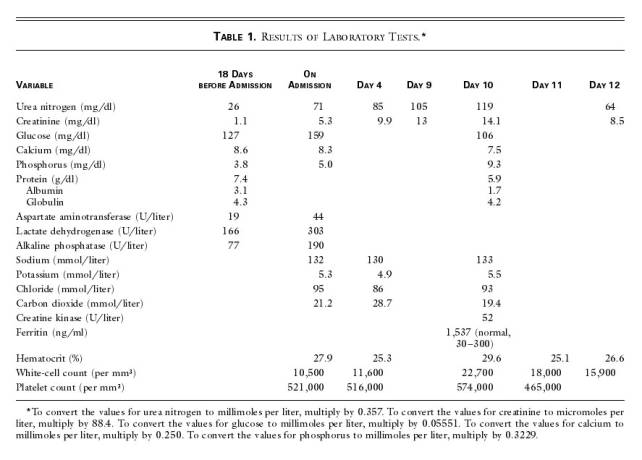
|
NEJM勉強会2003 第5回03/02/19 実施 Aプリント
担当: 唐沢康暉 (karasawa-tky@umin.ac.jp, http://www.karasawa.umin.jp/)
Case 4-2002:A 75-Year-Old Man with Acute Renal Failure Five Months after Cystoprostatectomy and Urethrectomy for Carcinoma
(Volume 346(5))
【患者】 75歳 男性 【主訴】 倦怠感,微熱,悪寒,食欲不振 【入院目的】 急性腎不全 【現病歴】 5ヶ月前に前立腺腺癌、尿道の乳頭状移行上皮癌に対し、 膀胱前立腺全摘術.尿道切除術を施行。回腸導管ileal conduitで尿路を再建した。術後、3週間、麻痺性イレウスとなった。(Table 1に入院18日前の検査データあり。) 入院2週間前、倦怠感,微熱, 悪寒、食欲不振を訴えたため、Ofloxacin 処方したが、散発的に服用しただけだったため、症状は改善しなかった。 外来で、尿路造影撮影法で、両側の腎臓がかすかな不透明化したのが判明し、その日に入院。(原文: a urographic examination disclosed faint opacification of the kidneys; there was no contrast material within the collecting systems and no hydronephrosis.)水腎症もなかった。(Figure 1) 【既往歴】 高血圧(enalapril:ACE阻害で加療中。) 乏尿や血尿(red urine)をnoteしたことがない 【生活歴】 alcohol (-), cigarettes (-) 少量のibuprofenを飲んでいた。 【入院時現症】appeared chronically ill <GENERAL STATUS & VITAL SIGNS> BW 健康時に比べ、体重が2kg減少した。BT 36.6℃, BP 120/70 mmHg, PR 64/min , RR 18/min <HEENT> [Eyes] conj: not anemic & not icteric, pupils: round & isocoric. [Ears & Nose] n.p. [Oral Cavity] tongue: n.p. [Neck] no goiter, bruit(-). His head, neck, and lungs were normal <LUNG> normal vesicular sound, no crackles. <HEART> Ⅰ→,Ⅱ→,Ⅲ(-),Ⅳ(-), 右胸骨縁に沿ってsystolic murmur(grade 1 ) <ABDOMEN> 右上腹部に限局した防御を伴った圧痛あり(反跳圧痛はない)。回腸瘻は正常のようで、ドレーンされた尿は濃縮されているが、血性ではない。 <EXTREMITIES> pitting edema(-) 【入院時検査所見】(Table 1を参照) <CBC> WBC 10.5×103/μl, Ht 27.9% , Plt 52.1×104/μl <CHEMISTRY> LDH 303 IU/l, AST 44 IU/l, ALP 190 IU/l, BUN 71mg/dl, Cr 5.3mg/dl, Na 132 mEq/l, K 5.3 mEq/l, Cl 95 mEq/l, cCa 8.3 mg/dl, iP 5.0 mg/dl, Glu 159mg/dl <COAGULATION> PT normal <U/A> Prot(+), RBC 20〜40 /HPF, WBC 5〜10/HPF.without casts or bacteria. (原文:the urine was trace positive for protein) PSA less than 0.5 μg per liter. Carbon dioxide 21.2 mmol/liter 【画像所見】 <ECG> normal <腹部・骨盤造影CT> intraabdominal massなし。 <腹部エコー> a normal common bile duct, a tiny polyp in the gallbladder, and no evidence of cholecystitis. 尿石症、水腎症の徴候なし。肝腎コントラスト ; the kidneys were hyperechoic in relation to the liver. <尿の細胞学的検査> degenerate epithelial cells あり。cancerous cellsだと考えられている。移行上皮細胞癌の再発の可能性があがった。血液、尿の培養では菌がなかった。 <99mTc-methylene diphosphonate scintigraphy> degenerative changes.あり,転移を示す所見はなし。 【入院中に行われた特殊検査】 回腸のループに逆行性に造影剤を注入したところ、欠損像はなく、腎杯、腎盂は正常。(原文:Retrograde examination of the ileal loop after the administration of contrast material revealed no filling defects; reflux of contrast material into both ureters showed that the calyces and pelves were normal.) 【入院後経過】 輸液(電解質)が行われ、トリメトプリム(抗菌薬)スルファメトキサゾール、オメプラゾール(抗潰瘍薬)が経口投与された。体温は入院してから8日間、37.7°Cから 38.8°C の間に上昇し、その間、BUN、creatinine levelsは、日々上昇した。右上腹部の圧痛:Tendernessは徐々に減少した。
メモ ・膀胱前立腺全摘術(膀胱,前立腺および精嚢腺を同時に摘出する手術方法) ・ileal conduit (回腸の遊離切片を膀胱から皮膚へ直結の機能として働かせること.導管内には両側尿管が接続され,導管の他端の内腔は皮膚に移植される.膀胱全摘の後または膀胱の正常の機能が失われたとき,膀胱より上部で尿路変更が必要となるため行われる). ・オフロキサシン, 合成抗菌剤(新キノロン系) ・ibuprofen:非ステロイド性消炎鎮痛薬 ・水腎症(片側または両側の腎盂および腎杯の拡張で,尿路の閉塞,膀胱尿管逆流の結果起こる ・回腸のループに逆行性に造影剤を注入したところ、欠損像はなく、腎杯、腎盂は正常。 Retrograde examination of the ileal loop after the administration of contrast material revealed no filling defects; reflux of contrast material into both ureters showed that the calyces and pelves were normal. ・両下肺野(over the lower third of both lung fields) ・A D-dimer test 2.0 〜 8.0 μg per milliliter(0.72 以下:FDPとの組み合わせにより一次・二次線溶亢進状態の鑑別に有用。線維素溶解療法時のモニターとしても有用な検査。 ) ・PT 14.7 s(control value of 12.2 seconds)外因系の凝固活性 対照±1.0秒 ・APTT( the partial-thromboplastin time) 65.4 seconds. 内因性凝固活性の指標 ・胸部X線写真の実質の不透明な部分に一致する、多発の血流欠損が見られた。multiple perfusion defects that corresponded to the regions of parenchymal opacities on the chest radiograph. 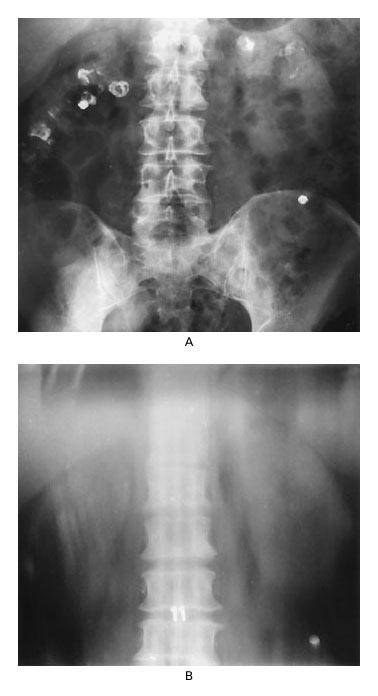
Figure 1. Radiologic Images Obtained after the Intravenous Administration of Contrast Material. ・On a radiograph obtained 90 minutes after the administration of contrast material (Panel A), the kidneys are faintly opacified, and the urinary tracts are not visible. In the right lower quadrant, contrast material is collecting in a bag over the patient's urinary ileal loop. The scattered opacities around the periphery of the radiograph indicate that there is residual enteric contrast material within colonic diverticula (Radiology): Figure 1A(A plain-film radiograph ) for a urographic study. The faint opacification in the right lower quadrant corresponds to urine collecting within the bag overlying the ostomy for the ileal loop. . A renal tomogram (Panel B), which was obtained 10 minutes later, shows that there is no contrast material in the intrarenal urinary tracts. Figure 1B(A tomogram) confirms that the kidneys are very faintly opacified, with no evidence of contrast material within the intrarenal collecting system. |